Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Getting Help for Plantar Fasciitis
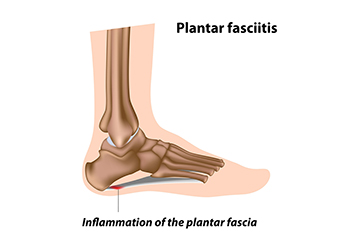
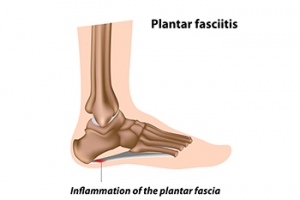
Plantar fasciitis is believed to be the most common complaint of heel pain. Plantar fasciitis is the inflammation of the plantar fascia, a broad band of tissue on the sole that supports the arch. This inflammation can make your heel hurt, swell, or turn red, particularly when getting out of bed in the morning. The causes of plantar fasciitis are varied, often stemming from factors like foot and calf tightness, weak foot muscles, or undue stress on the arch. Excessive running, wearing poorly fitted shoes, and some work actions can make the condition worse. Treatment focuses on addressing the root causes and reducing inflammation. It may involve wearing shoes with better arch support, changing shoe size, and moderating activities that strain the foot. Stretching and strengthening exercises, like towel curls, may help reduce symptoms. If you have developed plantar fasciitis, it is suggested that you make an appointment with a podiatrist who specializes in managing this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from DeCaro Total Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Common Sources of Heel Pain

Heel pain can be a real hindrance, affecting your daily life and mobility. Recognizing symptoms of heel pain helps you identify the cause and find relief. Plantar fasciitis is the most common complaint associated with heel pain. It often causes a sharp pain in the heel, especially in the morning. This condition occurs when the plantar fascia, the tissue connecting your heel bone to your toes, becomes inflamed. Achilles tendinitis results in pain in the back of the heel as the Achilles tendon, which connects the calf muscles to the heel bone, is torn and becomes inflamed. Heel spurs, bony growths on the underside of the heel bone, often accompany conditions like plantar fasciitis and may induce further pain. Bursitis, the inflammation of the bursa sacs around the heel, can lead to pain when walking or wearing tight-fitting shoes. Stress fractures, tiny cracks in the heel bone caused by repetitive stress, result in localized pain. If you're experiencing heel pain, it is suggested that you make an appointment with a podiatrist for an examination and a diagnosis. Then this medically trained foot doctor can formulate a personalized treatment plan to get you back on your feet pain-free.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of DeCaro Total Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
See Your Foot Specialist Regularly If You Work On Your Feet
Fungal Infections Affecting Toenails

Fungal nails, also known as onychomycosis, result from a fungal infection. This condition often leads to nail thickening and discoloration, along with the buildup of dead skin beneath the nail plate. Sometimes, the nail's shape can also change. Among fungal infections affecting the body, nail infections are particularly challenging to prevent and treat. Onychomycosis arises due to an overgrowth of fungi that thrive in warm, moist environments, such as locker rooms, public showers, and swimming pool areas. Typically, fungal growth begins at the nail's end and gradually spreads beneath it. Occasionally, chalky white patches may form on the nail's surface. As the infection progresses, yellowish or brownish discoloration becomes evident. The fungus can also cause damage to the nail's base, resulting in a thickening and altered shape. Treatment for fungal nail infections involves conservative, laser, and surgical approaches. Conservative treatment consists of using a topical medication applied like nail polish. Reinfection is a risk, and antifungal spray can be used inside shoes to treat any residual infection. Laser treatment for fungal nails is non-invasive. Surgical intervention is considered only if other treatments are not effective. If you have a fungal nail infection, it is strongly suggested that you make an appointment with a podiatrist to have your nails assessed and treatment administered that is right for you.
For more information about treatment, contact one of our podiatrists of DeCaro Total Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Let the Expert Treat Your Ingrown Toenails
Pain in the Ball of the Foot

Much of the body's weight is supported by the metatarsals, the long bones of the foot. When these bones become inflamed or irritated, it results in a condition known as metatarsalgia, or more commonly, pain in the ball of the foot. This causes varying degrees of discomfort that can disrupt daily activities. Metatarsalgia is often seen in active individuals, as a result of overuse and high-impact activities like running and jumping. Constrictive footwear and high heels that create pressure around the metatarsals can also contribute to ball of foot pain. Being overweight increases the risk of developing metatarsalgia. Symptoms include pain between the toes and the arch, which can intensify during movement and ease when resting. Numbness around the toes, especially the big toe and second toe, is common. Stretching and strengthening foot muscles, as well as the Achilles tendon, are essential for recovery from metatarsalgia. Proper footwear with arch support can aid in cushioning the foot's arch and providing relief. Surgical options might be considered if other pain management remedies prove inadequate. If you are experiencing pain in the ball of the foot on a continual basis, it is suggested that you make an appointment with a podiatrist for a full examination and discussion of treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from DeCaro Total Foot Care Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.