Common Foot Injuries From Running

Running frequently leads to foot injuries, including skin and toenail damage, plantar fasciitis, metatarsalgia, and peroneal tendonitis. Skin conditions like blisters and calluses often arise from friction and improper footwear. Toenail damage, including bruised or ingrown nails, can occur from repetitive impact and tight shoes. Plantar fasciitis, characterized by heel pain and inflammation of the foot's connective tissue, is common among runners. Metatarsalgia causes pain in the ball of the foot due to overuse or poor arch support. Peroneal tendonitis results in pain along the outer side of the ankle from excessive strain. To manage these conditions, rest and appropriate treatment are essential. Wearing well-fitted, supportive shoes, using orthotic inserts, and incorporating stretching and strengthening exercises can help prevent and relieve these common running-related injuries. If you have endured a foot or ankle injury while running, it is suggested that you visit a podiatrist who can effectively treat your foot condition.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact one of our podiatrists of DeCaro Total Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot And Ankle Injuries
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
Bunion Deformities
 A bunion, medically known as hallux valgus, is a deformity characterized by the misalignment of the big toe joint, causing the toe to lean toward the other toes and creating a noticeable bump on the side of the foot. This condition often results from a genetic predisposition, wearing tight or ill-fitting shoes, high heels, or conditions such as arthritis. Symptoms of a bunion can include pain, swelling, redness surrounding the affected joint, and difficulty walking. Over time, the deformity can worsen, leading to increased discomfort and mobility issues. Conservative treatments for bunions include wearing wide-toed shoes, using protective pads to reduce friction, wearing orthotics, and taking mild pain relievers. If conservative methods fail to provide relief, more invasive options can include corticosteroid injections to reduce inflammation or bunionectomy surgery to realign the bones, tendons, and ligaments. If you have a painful bunion, it is suggested that you schedule an appointment with a podiatrist for an accurate diagnosis and a personalized treatment plan.
A bunion, medically known as hallux valgus, is a deformity characterized by the misalignment of the big toe joint, causing the toe to lean toward the other toes and creating a noticeable bump on the side of the foot. This condition often results from a genetic predisposition, wearing tight or ill-fitting shoes, high heels, or conditions such as arthritis. Symptoms of a bunion can include pain, swelling, redness surrounding the affected joint, and difficulty walking. Over time, the deformity can worsen, leading to increased discomfort and mobility issues. Conservative treatments for bunions include wearing wide-toed shoes, using protective pads to reduce friction, wearing orthotics, and taking mild pain relievers. If conservative methods fail to provide relief, more invasive options can include corticosteroid injections to reduce inflammation or bunionectomy surgery to realign the bones, tendons, and ligaments. If you have a painful bunion, it is suggested that you schedule an appointment with a podiatrist for an accurate diagnosis and a personalized treatment plan.
If you are suffering from bunion pain, contact one of our podiatrists of DeCaro Total Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Factors for Seniors Seeking Exercise Shoes

Selecting the right exercise shoes is particularly important for seniors to ensure safety, comfort, and effectiveness during physical activity. Seniors should consider several factors when choosing footwear, such as the type of exercise they plan to do and the level of support required. The wear pattern on current shoes, foot shape, and arch support needs must also be weighed. High-impact activities such as running often call for shoes with more support, while activities like walking may require less. Analyzing the wear on old shoes can provide insights into your gait and help guide your choice. Foot shape and arch support are critical, as some feet have high arches, others are flat, and many fall inward or outward when standing. Exercise shoes should feel comfortable during extended wear and be aesthetically pleasing to encourage regular use. A podiatrist can assess your foot type, gait, and specific needs, in order to recommend the most suitable footwear to prevent injuries and enhance exercise performance. If you are looking for the right exercise shoes, it is suggested that you schedule an appointment with a podiatrist for guidance on options that are best for you to consider.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from DeCaro Total Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly and their Feet
While proper foot care is important for everybody, senior citizens have the tendency to be more susceptible to certain foot conditions. The elderly should therefore be well informed about any problems that may arise and about what they can do to properly avoid or treat them.
Some of the most common foot problems seniors are susceptible to include foot ulcers, ingrown toenails, fallen arches, and fungal nails. A foot ulcer is an open sore on the foot and can be a result of diabetes and decreased sensation in the feet. An ingrown toenail is defined as when the nail grows into the side of the toe. Fallen arches are indicated by the instep of the foot collapsing. A fungal nails is a condition that results in deformed and discolored toenails.
In order to avoid these conditions it is recommended that the feet be inspected by the patient on a regular basis. If these inspections are carried out routinely, there is a good likelihood that problems can be identified before they become severe, or can even be avoided altogether. If any abnormality is discovered, it is important that the individual consult a podiatrist for diagnosis and information on treatment options.
Proper foot hygiene is also important. Making sure that you always have clean, dry socks on can be a major deterrent to many different problems including bacterial infections, foot odor, and certain types of fungus. Wet feet are a major cause of many of these problems. If your socks get wet, it is important to change them. Walking around in wet socks may not only lead to various infections, but can irritate the skin and result in a number of various complications. Clean, dry feet are less likely to be affected by fungal and other infections.
As people age, the fat present on your feet begins to deteriorate. The protective nature of this fat keeps the feet healthy by providing a barrier between your bones and the ground. This also aids in giving the skin on the feet a certain amount of elasticity. This is one factor that causes elderly people to develop some serious foot issues. Foot moisturizers can be helpful to avoid certain problems associated with this. However, water-based moisturizers do not work as well for elderly people as they do for the young. Instead, it is more effective to use an emollient instead. An emollient is effective because it binds the water in the foot, keeping it from becoming absorbed too readily which will result in dry skin. Emollients also have a special property called occlusion, which provides a layer of oil on the skin. This layer prevents the foot from drying up and can be very effective in treating dry skin disorders. If you can keep the skin on your feet healthy, this will substantially reduce the number of foot problems you will encounter in old age.
Proper footwear is another way to keep feet healthy. Shoes that fit well and provide proper support help prevent ingrown toenails and fallen arches.
Certain medical conditions such as diabetes or poor blood circulation increase the risk for foot issues. For individuals with any of these conditions it is extremely important to conduct regular foot inspections to make sure that there are no sores or infections present.
Foot Pain May Be Linked to Falls in the Elderly
 Foot pain is a significant factor contributing to falls in seniors. Research indicates a link between severe foot pain and a higher incidence of recurrent falls in older adults. Conditions like arthritis, plantar fasciitis, bunions, and flat feet can cause pain that affects balance and gait. Flat feet, in particular, can lead to altered foot mechanics, increasing the risk of falling. A podiatrist can be instrumental in preventing falls by addressing these issues through regular foot examinations. This foot doctor can diagnose and treat foot conditions, as well as recommend supportive footwear and prescribe orthotic inserts. They can also provide pain management strategies and suggest personalized strength training and foot exercise programs that improve stability and mobility. If you are 65 years of age or older and have fallen in the last year as a result of foot pain, it is suggested that you schedule an appointment with a podiatrist for an exam and suggested fall prevention measures.
Foot pain is a significant factor contributing to falls in seniors. Research indicates a link between severe foot pain and a higher incidence of recurrent falls in older adults. Conditions like arthritis, plantar fasciitis, bunions, and flat feet can cause pain that affects balance and gait. Flat feet, in particular, can lead to altered foot mechanics, increasing the risk of falling. A podiatrist can be instrumental in preventing falls by addressing these issues through regular foot examinations. This foot doctor can diagnose and treat foot conditions, as well as recommend supportive footwear and prescribe orthotic inserts. They can also provide pain management strategies and suggest personalized strength training and foot exercise programs that improve stability and mobility. If you are 65 years of age or older and have fallen in the last year as a result of foot pain, it is suggested that you schedule an appointment with a podiatrist for an exam and suggested fall prevention measures.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from DeCaro Total Foot Care Center. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
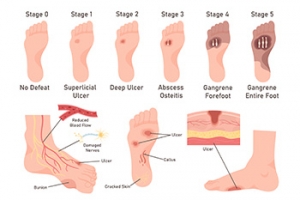
Debridement Methods for Diabetic Foot Ulcers
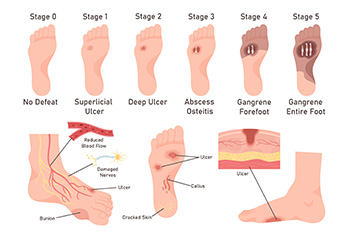
Debridement is a key procedure in managing diabetic foot ulcers, involving a podiatrist removing dead and infected tissue to promote healing and prevent infection spread. This process is vital because the buildup of necrotic tissue can obscure the true extent of the ulcer. There are several methods of debridement. Surgical debridement involves a podiatrist using tools like scalpels to precisely remove dead tissue, often performed at the bedside or in an operating room for more severe cases. Mechanical debridement employs saline-soaked pads that adhere to and remove dead tissue upon removal, though this can be painful and may also disturb healthy tissue. Chemical debridement uses enzymes to dissolve dead material. Biological debridement, utilizing maggots, effectively cleanses wounds by consuming only dead tissue. Before any debridement, the podiatrist will assess the patient’s overall health, and the wound will be cleaned with a saline solution. If you have diabetic foot ulcers, it is suggested that you make a podiatrist a part of your medical team for expert wound care options.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from DeCaro Total Foot Care Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in West Hatfield, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.